After the Department of Health's presentation to parliament and the Medium-Term Budget Statement, NHI is back in the news. Let's try to get a grip on it.
Change is inevitable
The healthcare system in South Africa (SA) is profoundly unequal, with affluent people accessing the best in the world while the poor are faced with hours-long queues for monthly medicine. Private patients continue to face increases that outstrip inflation by a margin, while the public health system is under huge strain. There is no dispute that this needs to change.
The problem, and attempts at solutions, are not new, dating back to the dawn of democracy.
Reform
Health reform in SA started in 1994 with free care for mothers and children under 6. Primary healthcare was prioritised, and a massive clinic-building drive was undertaken.
In 1995, an NHI inquiry proposed a universal basic primary healthcare package in the public sector and retention of individual choice to use private providers, but within a regulated insurance market.
This resulted in the 1999 Medical Schemes Act, 131 of 1998, which introduced community ratings, open enrolment, and prescribed minimum benefits that all schemes were required to cover in full.
In 2002, the Taylor Committee proposed a 4-phase process to achieve universal contributory health cover 'based on multiple funds and a public sector contributory environment'. The idea was to expand medical scheme coverage as part of the transition to universal health insurance. 'The objective would be to achieve jointly what each cannot achieve alone.'
However, in 2007 this incremental approach to building a health system that combined public and private sectors was reversed at the Polokwane Conference, where Jacob Zuma was elected ANC president. Policy switched to a single state-funded NHI. The 2019 NHI Bill, signed into law in 2024, is the outcome of that shift. (For an excellent overview of the reforms since 1994 and more details on the history, see Donaldson and Kahn, referenced below.)
Promise of the same care for all
NHI envisages a single state-run fund to pay for health services for the entire population and a diminished role for medical schemes. It would be funded by pooling all current public and private medical expenditure, plus extra taxes.
The vision is clear: all citizens must have access to the same level of benefits. But the department has studiously avoided telling us what those benefits would be and, importantly, what it would cost. There is only the suggestion that it would be the same as medical aids currently offer. The deputy minister of health, for example, has said that civil servants should not worry about losing their medical aid membership, because the NHI will pay for their health services. In October, the minister of health told a parliamentary committee that he finds lower-cost medical aids offering fewer benefits 'offensive'.
The numbers tell a different story
Simple arithmetic suggests that it is impossible to extend the level of healthcare that medical aid members currently enjoy to all South Africans without substantial additional funding. There are 9-million beneficiaries of medical aid. The total population is about 64-million. Either taxes will have to increase dramatically, or the level of services covered by the NHI will have to drop dramatically.
If the fund comprises only pooled current expenditure on public and private healthcare, spending per beneficiary will have to drop by about two-thirds, or 66.7%, of what current medical aid members enjoy. Adrian Gore from Discovery has put the number at 70%. Huge tax increases will be needed to take treatment levels back up to 100%.
Going beyond simple arithmetic, Genesis Analytics undertook a study commissioned by The Health Funders Association and found. It found that the NHI would cost an estimated R940-billion a year – R400-billion more than SA's combined public and private healthcare expenditure of R530-billion in 2022 – and would require that the average rate of personal income tax more than double from 21.3% to 47.5%.
Groups as diverse as the Progressive Health Forum, the Universal Healthcare Access Coalition, the Health Funders Association, business groups and professional bodies have warned that the idea that NHI can cover all medical benefits for the entire nation is not fiscally possible. Says Aslam Dasoo, Convenor of the Progressive Health Forum: ''the NHI is fiscally … unimplementable. There is no feasible scenario in which a single tax-financed fund can provide all the cover for the entire population.''
The numbers are unforgiving. They present a stark, unpleasant choice: either higher taxes or lower levels of service.
Alternatives are available
As the Health Department worked single-mindedly towards the NHI, several alternatives were proposed.
In 2014, the Competition Commission initiated the Health Market Inquiry (HMI) to identify potential barriers to competition that contribute to ever-rising costs in the private healthcare sector. Its 2019 final report provided a detailed and systematic assessment of private healthcare. It provided an opportunity to revert to a phased implementation of health reform, building on the strengths of both the public and private sectors.
In 2017, the High-Level Panel Review of SA Legislation, chaired by former president Kgalema Motlanthe, proposed a 3-tier model for health combining private sector medical schemes, government employees' medical schemes and an NHI scheme for those not covered.
In 2024, the Universal Healthcare Access Coalition proposed mandatory medical scheme membership for higher-income individuals, accompanied by mechanisms to pool risks between schemes, converting the current tax benefit into an income-related contribution subsidy and a new public scheme to compete with private schemes.
To strengthen the public sector, the coalition proposed that hospital authorities should have more autonomy over procurement, appointments, and operational decisions, and be overseen by independent hospital boards. The Tembisa story underscores the value of this recommendation.
It also called on the government to initiate discussions with neighbouring states to cover the cost of their citizens' use of SA public health services – a prescient proposal, given the ongoing protests about foreigners using SA health facilities.
In 2025 the Health Funders Association (HFA) proposed another alternative that it calls NHI+. Under this model, NHI and medical schemes will cover a common benefit package delivered by public and private providers, and all taxpayers will contribute to the NHI Fund – either directly or via mandatory contributions to medical schemes. As with the Healthcare Coalition's proposals, there will be risk equalisation between funds, and redistributive arrangements will see medical schemes subsidising the NHI Fund for the common benefit package.
The key difference
The key difference between NHI and the above alternatives is that the alternatives steer away from establishing a state-run monopoly, instead proposing hybrid systems relying on both the public and private sectors. In fact, health financing is a hybrid mix of systems in all advanced economies (Donaldson & Kahn).
Even in Britain, where the National Health Service has been in existence for 77 years and is a national institution, 10% to 12% of the population hold private medical insurance. The famous '30 baht' national scheme in Thailand is not a single monolithic fund but one of 3 main public insurance funds operating in parallel. Therefore, having 1 state-run monopoly fund is truly an outlier.
This key difference is encapsulated in section 33 of the NHI Act, which prohibits medical aid schemes from covering benefits that the NHI already covers. Without that section, a hybrid system as proposed in all the alternatives above can develop under the Act.
Regulation
Part of any alternative is the regulation of the private sector, as recommended by the HMI as early as 2019. Business for South Africa calculates that savings of 20% in private medical insurance can be achieved if the HMI proposals are implemented.
Prospect of change
There is a faction within the ANC and Health Department that is fiercely committed to the single-fund NHI model. Might other realities force a shift?
Court challenges
The Act has been passed, but legal challenges have stalled implementation. Eight court cases are currently winding their way through the system.
In one of the cases, the High Court in March 2024 declared directives in the Act stipulating where doctors may work unconstitutional. The decision was appealed, and the case was heard in September. Judgment is awaited.
Adverse court rulings will force a rethink by the health authorities. In fact, there are suggestions that this is a deliberate political tactic: to wait for whole or parts of the NHI Act to be struck down, allowing for a redesign to take place.
Politics – conspicuous silence
In January, the DA declared a dispute with its GNU partner, the ANC, on NHI. In February, Planning, Monitoring, and Evaluation Minister Maropene Ramokgopa reportedly disclosed to News24 that the two parties had reached a compromise, enabling sections in the NHI Act that threaten the existence of medical aids, such as section 33, to be amended.
Enquiries with the DA confirm that such a compromise was indeed reached. However, Health Minister Motsoaledi promptly denied that section 33 would be changed, and since then both the ANC and DA have remained quiet on the matter.
At the same time, news reports emerged indicating that the ANC was considering proposals for all working citizens to belong to a medical aid, that the NHI fund will compete with private medical schemes, and that unemployed people will still make use of state hospitals. This proposal aligns closely with the Universal Healthcare Coalition's proposals. Again, it was denied by Health Minister Motsoaledi, and all talk of such proposals went quiet. Is the silence part of a tactic to wait for the court rulings to be made and then go back to the drawing board?
Follow the money – not much of it
At a press conference accompanying his Medium-Term Budget Statement, the finance minister was quite emphatic that the NHI plan to phase out medical aid tax credits is 'an attack on the middle class'. He was decidedly not keen to remove tax credits from the same people who are paying the bulk of personal income tax without an alternative.
It is clear that 'an alternative' is not going to come from the Budget. The May Budget provided for an increase in health expenditure of 5.9% per annum over 3 years, adding a total of R30-billion over the period. In the Medium-Term Budget Statement in November, the number was reduced to 3.9% p.a., adding a total of R36.6-billion over 4 years.
NHI is allocated R9.9-billion to develop a patient information system, a centralised chronic medicine dispensing and distribution system, and a medicine stock surveillance system. This will improve the health infrastructure, which is very far away from funding NHI services as envisioned.
Connecting all the above, it is safe to say that Minister Motsoaledi and the Department of Health stand quite isolated within the government, and perhaps even within the ANC as a whole.
Insiders versus outsiders
The insider/outsider divide may reinforce their isolation.
Most civil servants belong to the Government Employees Medical Services, while senior officials have more flexibility in their choice of scheme. Under the Act as it stands, these benefits will be terminated, and the funds will be absorbed into the common NHI fund. COSATU unions are strong supporters of the NHI, while the Public Servants Association is strongly opposed, and others take a wait-and-see attitude. In a classic case of insiders versus outsiders, union members are unlikely to agree to exchange their current benefits for the uncertainty of NHI treatment.
This issue is even more pertinent because this change (all civil servants switching to NHI) is foreseen in year 7 of the 15-year conversion to NHI. Civil servants will therefore lose their existing benefits before the NHI is fully operational. Expect massive pushback.
Pushback may also be fuelled by discrimination between civil servants.
Section 2 of the NHI Act excludes members of the SA Defence Force, State Security Agency and SA Police Service from the Act. The military runs its own hospitals, but why that expenditure is not also reprioritised into the NHI Fund and why military hospitals cannot become service providers to the NHI like other hospitals is not clear. And why are the spies privileged? Police officers are members of POLMED and will continue to enjoy their medical aid cover.
Other civil service members may not take kindly to this discrimination favouring some.
Creating a new reality
In August, the Motor Industries Bargaining Council concluded an agreement with NUMSA to introduce a primary healthcare benefit for garage workers. This is a first in the industry and a welcome breakthrough for low-paid workers in that industry.
Unions are unlikely to wait 15 years for NHI. They will negotiate agreements like this one, which improve medical cover for their members. That can shift the balance of power around NHI considerably over the next decade.
A swerve to realism
In the presentation made to parliament in the last week of October, the Department of Health outlined a 15-year implementation timeline for NHI. That far exceeds the deadlines set in the Act and indicates a swerve to realism on the part of the planners.
Clearly, NHI is not going to be a 'Big Bang' event, but an incremental process. This has been admitted by the minister in public and in court documents. (The presentation was a confusing tangle of assumptions, omissions and internal contradictions, but that is another story.)
The upside to a 15-year implementation plan is that a lot of water will flow under the NHI bridge during that time.
For one, economic growth can significantly impact the country's ability to finance healthcare. More time also allows for better alternatives to be implemented. More big swerves can occur in 15 years.
One is struck, however, by the irony of NHI now pursuing an incremental path, while it scuppered the incremental reform of healthcare taking place slowly but surely before 2007.
So What?
The healthcare system is unsustainable and must change.
The NHI in its current form is 'fiscally and institutionally unimplementable', in the words of Aslam Dasoo of the Progressive Health Forum.
From all the evidence, a hybrid system in which NHI exists alongside private funds is the better route to wider and better healthcare.
Regulation of the private sector to curb excessive cost rises is an essential part of reform. The implementation of the HMI recommendations can render savings of up to 20%.
Both the Department of Health and the 'no-NHI-at-all-cost' camps must take a step back and plot a different route to the ultimate aim – better healthcare for all.
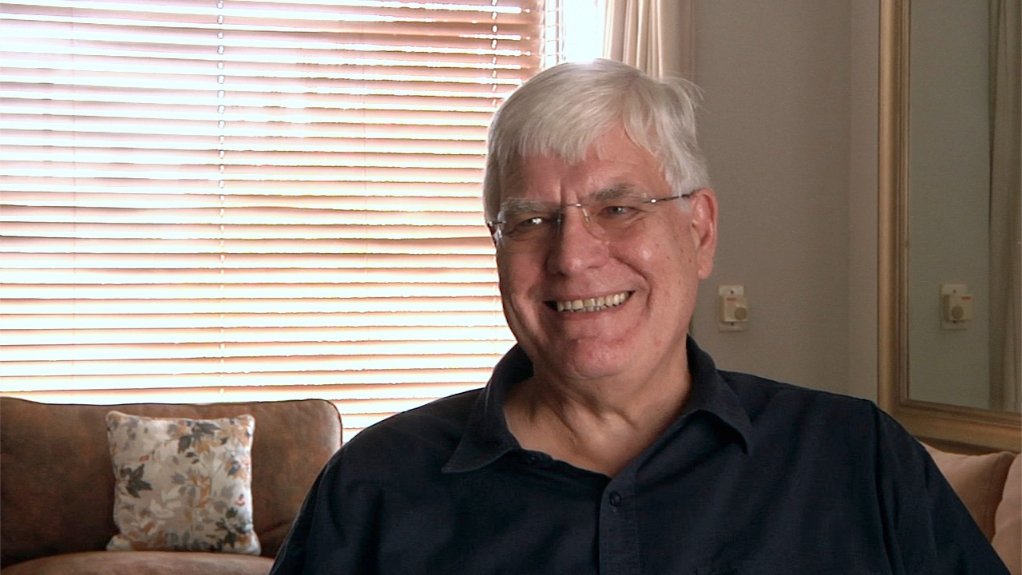
Written by JP Landman, Political & Trend Analyst
Sources:
Andrew Donaldson & Tamar Kahn, Health Policy in South Africa – From 1994 to now, Policy Paper 32, ERSA, 2025.
National Treasury, Budget Review 2025.
National Treasury, Medium Term Budget Policy Statement 2025.
Department of Health, Presentation to the Standing Committee on Appropriations of Parliament, October 2025.
Business for South Africa and BUSA, Presentation on NHI, November 2023.
A variety of news articles from different media.
EMAIL THIS ARTICLE SAVE THIS ARTICLE ARTICLE ENQUIRY FEEDBACK
To subscribe email subscriptions@creamermedia.co.za or click here
To advertise email advertising@creamermedia.co.za or click here